The American Urological Association, AUA, tells us that the cause of Interstitial Cystitis/Bladder Pain Syndrome, IC/BPS, is unknown and that there is no cure. However, hundreds of patients and some doctors tell us otherwise.
This research, on a urological diagnosis and treatment of interstitial cystitis/bladder pain syndrome, IC/BPS, attempts to answer three questions:
- What does the American Urological Association, AUA, recommend to 22,000 urologists in America as the best treatment for a diagnosis of interstitial cystitis/bladder pain syndrome (IC/BPS)? (This diagnosis is for symptoms of urgency and frequency and “bladder pain.”) Keep in mind that urologists all over the world follow the treatment guidelines the AUA recommends, affecting millions more women, and some men.
- Does this “treatment” improve patient symptoms? In a word, no.
- Are there known causes and cures for the symptoms urologists call IC/BPS, and what are they?
These 3 questions will be answered in 3 sections, each section with more information.
Section one:
Question 1. What does the American Urological Association, AUA, recommend to 22,000 urologists in America as the best treatment for a diagnosis of interstitial cystitis/bladder pain syndrome (IC/BPS)?
• The AUA recommends dozens of trial and error “procedures” for a diagnosis of IC/BPS. In 2009, with the help of a billing office in a hospital in New York, I discovered that these “procedures” are in fact surgeries, with surgical CPT codes. You have a legal right to your medical records, and if the CPT codes aren’t included, you can ask to see them.
As the surgeries are “trial and error,” they often amount to dozens of surgeries, and patients are told that eventually something will work, and improve their symptoms.
When you agree to these surgeries, you are also agreeing to take the antibiotics that go with them – all surgeries require antibiotics, to avoid infection.
The question is, are these surgeries effective? All surgeries are harmful, and if the patient is not expected to be much more benefitted than harmed by the surgery, the surgery is unethical. Because antibiotics can cause many diseases, it’s best to avoid surgeries with no benefit. (footnote 5)
The surgeries recommended are: hydrodistentions of the bladder, instillations of chemicals like DMSO (a wood solvent), Heparin and/or Lidocaine, implantation of neuromodulation devices under the skin, Intradetrusor botulinum toxin A (Botox), Cyclosporine A, and finally “diversion” of urine, which means either removal of the entire bladder (cystectomy) or part of the bladder.
Most of these surgeries are each done multiple times. You’ll see this in James’, Susie’s and Anne’s stories in theLetter to the AUA, that Dr. Kavaler and I sent to 3 committees of the AUA in 2013.
Practice Guidelines can be viewed at
http://www.auanet.org/guidelines/interstitial-cystitis/bladder-pain-syndrome-(2011-amended-2014) For a summary, click to open: Executive Summary
There are also many other surgeries done, which are not in the Practice Guidelines, such as “dilation of the urethra.” This surgery has been done since 1917, at major Universities and hospitals all over the country, to many millions of women, and even female infants and children. And to millions more in other countries. Once started, dilation is often done for a whole lifetime. It does not appear in the Practice Guidelines, nor is it “recommended against.” Likely because dilation is very profitable, the last I heard it is reimbursed at $600. per dilation, done quickly and easily in the urologist’s office. Does it help patients?
Question 2: Does this “treatment” improve patient symptoms? In a word, no.
• Some doctors would call the American Urological Association’s (AUA) Practice Guidelines (suggested treatment) for IC/BPS “Type II Medical Malpractice,” that is “..doing something to patients … that was not needed in the first place.” This kind of malpractice is at present a scourge in all medical specialties.” (footnote 1) See Dr. Nortin M. Hadler’s books: Last Well Person, and Worried Sick.
Type II Medical Malpractice is one form of “iatrogenic harm,” or harm caused by the doctor.
To understand what Type II Medical Malpractice can do to a patient’s life, you might start reading Dr. Elizabeth Kavaler’s and my Letter to the AUA, both the text and 3 patient stories. It’s long, and it’s worth every minute you spend reading it. I strongly recommend that you read James', Susie’s and Anne’s stories, pages 33-36, 36-44, and 44-58, respectively. The real cause of James’ so-called IC was actually pelvic floor muscle dysfunction, PFMD, not a bladder problem and physical therapy for PFMD gave him great relief from severe pain. Susie had mild urgency and frequency as a child. Urologists diagnosed her with IC/BPS and this led to dozens of surgeries, and the antibiotics that go with those surgeries, recommended by the AUA. The end result was removal of her bladder and cancer, among many other health problems. She has given us her story, a warning, “so that other people won’t have to go through what I went through.” Anne’s story is also representative of so many issues that we all face with the AUA Practice Guidelines, including diagnosis with IC/BPS, 31 very painful surgeries and much more difficulty in being the kind of wife and mother she had been before the diagnosis and “treatment” of so-called IC/BPS. Eventually, after 16 years of unnecessary surgeries, antibiotics and suffering, the mother of Anne’s daughter’s roommate had the answer – the correct diagnosis of Anne’s extreme pain. The hysterectomy Anne had had just before the so-called IC symptoms began, had caused her pain, and physical therapy for myofascial stricture finally relieved her of 95% of her pain. This summary of these 3 stories is not enough – there is so much information in these stories.
• The consequences of a diagnosis of IC/BPS, and the AUA treatment for this diagnosis, are that dozens of trial and error surgeries cause a great deal of harm to the patients; surgeries are always harmful, and when ineffective also unethical. ( footnote 3 )
The AUA “Practice Guidelines,” still recommend removal of the bladder as a “last resort.” Sometimes there is so much pain that urologists tell a patient that the only thing they have left to offer is removal of the bladder. The patient believes this might stop the pain – since they’ve been told that the cause of their pain is their bladder (interstitial cystitis) for months or years. Removal of the bladder can make it much worse. The surgeries, for example 3 hour hydrodistentions under high pressure, can cause the bladder to shrink to almost no capacity. Again some urologists suggest removal of the bladder.
What happens after the bladder is removed?: Please read Susie’s story.
• Is dilation of the urethra effective? The theory was that women were having bladder infections because our urethras are “too narrow,” and need to be dilated. However, dilations are a surgery, and scar tissue forms, narrowing the urethra more and more with each dilation. Once started, dilation often continues for a lifetime. Eventually more dilations are needed in order to keep the urethra open and allow the woman to urinate. Dilations were also done, from the 1960s on, to female infants and children.
“Dilation” of the urethra continues today, even though it has been scientifically proven that a “narrow urethra” is extremely rare and only caused by trauma. (footnote 2) Urethras are flexible and almost all of them allow the bladder to empty and “narrow urethras” are not responsible for bladder infections. Dilation is very profitable, the last I heard $600. per dilation, done in the urologist’s office. It appears that dilation is clearly Type II Medical Malpractice, something that shouldn’t have been done in the first place.
The AUA assumption doing surgeries on the bladder will somehow improve patient symptoms also precludes the discovery of a cure, or real improvement of symptoms. Not looking “beyond the bladder” for the causes of symptoms, makes a cure impossible. A holistic approach can often provide a cure. We have many examples in Section 2 of this document.
• One urologist, Dr. Christopher Payne, (Stanford Professor Emeritus) gave three lectures at urological meetings in 2017, in which he said that the “Emperor has no clothes;” the “Emperor,” is the AUA Guidelines for treatment of so-called IC/BPS; the surgeries on the bladder recommended by the AUA are not effective for 90% of people diagnosed with IC/BPS.
As with every profession, in medicine there are good actors and very bad actors. I do not intend to paint all urologists, or all doctors, with a broad brush. However, the AUA, I believe, should be investigated by all our health care institutions, exactly because the Practice Guidelines are Type II Medical Malpractice.
• Question 3. Are there known causes and cures for the symptoms urologists call IC/BPS, and what are they?
Urologists and other doctors, like Dr. Payne, and dozens of patients tell us that there are many causes of the symptoms of chronic urgency and frequency and “bladder pain.” In fact, if we do look “beyond the bladder,” it’s clear that the symptoms the AUA call “bladder pain,” can come from other organs in the pelvis, and even from previous pelvic surgeries on other organs. For example, many of Dr. Payne’s patients are treated for myofascial stricture, with physical therapy, myofascial stricture release, MSR, for this condition. As many as 44% of women diagnosed with IC/BPS had a hysterectomy just before the onset of so-called IC symptoms, and their symptoms were actually caused by damage to myofascial tissue in the pelvis from the hysterectomy. This is a situation very well explained by Anne, in our Letter to the AUA, pages 44-58.
In addition to Anne, and two other people, whose stories are in our Letter to the AUA, I have interviewed dozens of people diagnosed with IC/BPS. When urologists didn’t help them, they went to other health care providers. Some were correctly diagnosed (the real cause of symptoms found), got the appropriate treatment, and were cured or got real relief from symptoms. Both James’ and Anne’s stories illustrate this, in our Letter to the AUA, pages 33-36 and pages 44-58. In Section 2 of this document, you’ll see many more stories of people who got the right diagnosis and treatment.
________________________________
Time out - what is our Letter to the AUA, and what is the evidence we use to answer these three questions? This evidence is:
• First, there is evidence from an online survey by myself and my urologist at the time, Dr. Elizabeth Kavaler. We decided to do an online survey of people diagnosed with IC/BPS, asking them whether the treatment benefitted them, made their symptoms worse, or had no effect and we were astonished to get 750 responses within weeks. These results were analyzed, and published in the Journal UROLOGY, in 2008:
https://www.goldjournal.net/article/S0090-4295(07)02143-7/fulltext
Then, in 2017, Dr. J Curtis Nickel, President of the Canadian Urological Association, CUA, borrowed the data from the total number of completed surveys, 1628 women, and published the results in the CANADIAN JOURNAL OF UROLOGY:
https://www.cuaj.ca/index.php/journal/article/view/4505
• Second, there is evidence from the medical literature in Dr. Kavaler’s and my Letter to the AUA, (see 7 pages of footnotes, pages 16-22) The medical literature about the surgeries recommended by the AUA for IC/BPS is unethical, the Practice Guidelines extremely harmful and quality improvement and patient safety dependent on the knowledge and character of each urologist – in general, quality of care is dependent on the urologist not doing these very profitable surgeries/antibiotics. There are 60 references to the harm from antibiotics that go with the dozens of ineffective and harmful surgeries the AUA recommends. And pages 9 and 10, Dr. Brookoff’s words, explain how the surgeries damage people’s bodies. Again, please see the 3 patient stories: James, pages 33-36, Susie, pages 36-44, and Anne, pages 44-58. It took many hours of these people’s time to give us these stories, and if you wish to thank them, email me and I’ll forward your thank you to them: zakariasen@verizon.net.
• The third kind of evidence we have used is the best evidence that urologists have regarding the efficacy of the treatment they recommend: the ICDB Study and many random controlled trials (RCTs), ICCTG and ICCRN trials done with the help of the National Institutes of Health (NIH), the NIDDK Division. These trials are almost impossible to find online, likely because the results contradict the Practice Guidelines. That is, only one trial, physical therapy for myofascial stricture, was successful, according to Dr. Payne at the 2010 convention of the AUA. Again, none of the trials of surgeries were successful in relieving symptoms of patients.
• The fourth kind of evidence comes from my interviews with dozens of patients diagnosed with IC/BPS, and conversations by email with several urologists and other doctors.
• Finally, I use other medical evidence, such as the International Human Microbiome Project, Dr. Martin Blaser’s research, about the effects of overuse of antibiotics, which is part of this Project.
________________________________
Section 2: Read more information about these three questions:
Question 1. What does the American Urological Association, AUA, recommend to 22,000 urologists in America as the best treatment for a diagnosis of interstitial cystitis/bladder pain syndrome (IC/BPS)? Again, dozens of trial and error surgeries, which the AUA claims eventually improve patient symptoms.
Question 2. Do these surgeries and antibiotics improve patient symptoms?
• THE SURVEY TELLS US:
• UROLOGY (the American urology Journal) January, 2008: “Patient Perceived Outcomes of Treatments Used for Interstitial Cystitis.” In short, the first 750 surveys submitted by patients, up to 2006, told us that the surgeries recommended by the AUA weren’t improving their symptoms, and only 3 of the 61 pharmaceuticals were somewhat beneficial for a some patients. The Journal UROLOGY,
https://www.goldjournal.net/article/S0090-4295(07)02143-7/fulltext
• Dr. J Curtis Nickel, President of the Canadian Urological Association, CUA, and his team borrowed the data from our survey, the data from all , 1628 submitted surveys and in 2017 published the results:
https://www.cuaj.ca/index.php/journal/article/view/4505
“Conclusions: There is a disconnect between real-world patient perceived effectiveness of IC/BPS treatments compared to the efficacy reported from clinical trial data and subsequent guidelines developed from this efficacy data. Optimal therapy must include the best evidence from clinical research, but should also include real-life clinical practice implementation and effectiveness.”
In other words, there is a disconnect between what patients say, that the treatment is ineffective, and what urologists say, which is that the treatment is effective.
• The National Women’s Health Network Newsletter, 2009, my story (Kay), and a summation of survey results:
https://www.nwhn.org/the-treatment-and-mistreatment-of-chronic-urgency-and-frequency-gathering-womens-experiences-about-interstitial-cystitis/
• The medical literature cited in our Letter to the AUA, the Judicial and Ethics Committee, the Practice Guidelines Committee and the Quality Improvement & Patient Safety Committee, tells us that the surgeries/antibiotics recommended by the AUA for IC/BPS are :
1. ineffective,
2. harmful,
3. there are alternative medical diagnoses and treatments which are successful and noninvasive, according to patients,
4. the treatment for IC/PBS is not evidence based, nor is there realistic disclosure in two definitive documents: Practice Guidelines, 2011, and in Campbell-Walsh Urology, 2011 and virtually no disclosure to patients, about the nature, benefit-to-harm ratio and alternatives to urological treatment,
5. and finally, this treatment paradigm is a breach of Patients’ Rights and human rights; this century and a half old tradition of multiple surgeries for each patient should no longer be offered patients.
I am aware that there is some strong language in this letter. I have thought about the wisdom of this at length. I am asking you to reconsider a century and a half old medical tradition. I have no idea what the intentions have been as no one can read another’s heart. But a lot of damage to millions of women, children and some men has been done.
Actually, one can read Dr. Brookoff’s heart, a kind doctor very concerned for his patients, on pages 9-10 of this Letter to the AUA.
Please read the Letter to the AUA at any of these links:
• Published on our original website, www.cystitispatientsurvey.com, Letter_to_AUA-cystitispatientsurvey.pdf
• Windsor Square, an online newspaper, published our Letter to the AUA because the Editor had a friend who had suffered the “treatment” recommended by the AUA:
http://www.windsorsquare.ca/archives/2013/do-you-suffer-from-pelvic-pain/53922
http://www.scribd.com/doc/147414544/Research-into-the-treatment-for-interstitial-cystitis-painful-bladder-syndrome
• Our Bodies Ourselves:
http://www.ourbodiesourselves.org/cms/assets/uploads/2014/04/Zakariasen_ltr_to_AUA_4.18.13.pdf
• The urological evidence tells us:
• The Interstitial Cystitis Data Base study, concluded that “…no current treatments have a significant impact on symptoms with time,” making the Practice Guidelines of the AUA an “irrational” treatment.(footnote 4)
See Rovner, Eric , KJ Propert, et. al “Treatments used in Women with Interstitial Cystitis: The Interstitial Cystitis Data Base Study Experience” UROLOGY 56 (6), 2000.
https://repository.niddk.nih.gov/studies/icdb/?query=None
“Outcome: The study found that initial analyses of patient data supported the clinical observation that IC is a chronic disease and showed that no current treatments had a significant impact on symptoms over time.”
https://www.ncbi.nlm.nih.gov/pubmed/11113737
• There were also numerous random controlled trials (RCTs) done with the help of research scientists at our National Institutes of Health,, NIH, the NIDDK division. As Dr. Payne said at the 2010 AUA Convention, only one trial was successful, the one on myofascial pain and treatment with myofascial stricture release physical therapy. Only physical therapy in general is mentioned in the Guidelines, not MSR in specific. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4708560/ See Anne’s story in our Letter to the AUA, pages 44-58. She explains well what myofascial pain is and how the physical therapy works.
• Dr. Christopher Payne, Professor Emeritus of Urology at Stanford, gave lectures at three urological meetings in 2017:
Dr. Payne says that a 2007 review of 203 biopsies of bladders, (Leihy, RF et al, J UROLOGY, 2007:177:142-148) indicates that 90% of people diagnosed with IC do not have a bladder disease and their symptoms may be curable.
Some people diagnosed with IC have Hunner’s ulcers or cancer in their bladder, and the appropriate surgeries will help them.
In Dr. Payne’s words, “The Emperor Has no Clothes.”
https://www.ic-network.com/dr-chris-payne-presentation-icbps-aua-2017
In Dr. Payne’s private practice, the majority of his patients have myofascial issues, for which he recommends myofascial physical therapy, and if that doesn’t bring progressive relief, other therapies.
Dr. Payne does not say this, but one study does indicate that as many as 45% of women diagnosed may have so-called IC symptoms which are actually caused by damage to the myofascial tissue during a hysterectomy. In this case, the so-called IC symptoms begin right after a hysterectomy. (footnote 12)
• The International Human Microbiome Project tells us:
When you agree to dozens of surgeries (often called “procedures), you are also agreeing to the dozens of antibiotics that go with these surgeries. Without antibiotics, the surgeries can cause infection.
What the International Human Microbiome Project has shown is that there are consequences also, from antibiotics: according to Dr. Martin Blaser, of the International Human Microbiome Project, overuse of antibiotics has caused many “modern plagues,” which include “… obesity, asthma, allergies, diabetes, and certain forms of cancer.” (Cancer – see Susie’s story, in the Letter to the AUA, pages 36-43) Blaser’s new book is Missing Microbes; How the Overuse of Antibiotics is Fueling Our Modern Plagues , 2014. Dr. Blaser’s book is very readable. It’s not a novel, but it is a thriller, and a recipe for survival. Blaser:
http://martinblaser.com/ (footnote 3)
In other words, when you agree to a surgery, you want to make sure that that surgery will be of much more benefit to you than harm. (footnote 3)
It appears that the dozens of surgeries recommended by the AUA are not effective – there is no benefit. And there is severe harm both from the surgeries and antibiotics.
If the surgeries are ineffective, both the surgeries and the antibiotics are, in medical language, “unnecessary,” and should not be used. They are one example of Type II Medical Malpractice – doing something to the patient that wasn’t necessary in the first place. (footnote 1)
The International Human Microbiome Project,is relatively new. But doctors have known since the first commercial use of antibiotics in the 1940s that antibiotics cause an overgrowth of a fungus called Candida albicans infection, which has many serious, painful consequences. (footnote 5)
Question 3. Are there known causes and cures for the symptoms urologists call IC/BPS, and what are they?
The AUA tells us that two things should be ruled out before a diagnosis of IC/BPS, Hunner’s ulcers and cancer in the bladder. Surgeries in these two cases can provide a lot of relief. However, two women have told me recently that after seeing many urologists, over many years, all these urologists failed to see the ulcers in their bladder. Finally, these women went to uologists who spotted the ulcers, the surgery was successful and stopped years of chronic, severe pain. You may need a urologist who is carefully looking for Hunner’s ulcers and cancer, and who is willing to put in writing how long and under what pressure his or her hydrodistentions are done. The AUA recommends against 3 hour hydrodistentions – is that enough to prevent this practice? I know of two clinics in New England that do 3 hour hydrodistentions at high pressure, and then likely take the bladders out because this kind of hydrodistention can cause the bladder to shrink to almost no capacity.
Over the years I have interviewed dozens of people, and asked them if a doctor or other person had finally discovered the real cause/s of their symptoms and given them treatment that was effective – a cure or significant relief of symptoms. All of these people were diagnosed with IC/BPS, but the causes were almost always “beyond the bladder,” which means that the bladder is not the cause of symptoms.
The following is a list of what these people told me about the real causes of their symptoms, when they were lucky enough to find the right health care provider – or in Anne’s case, the mother of her daughter’s roommate in college! Anne, whose story is here .
You might take this list of some of the causes of urgency and frequency and pelvic pain with you to your family doctor or any other doctor who is willing to test you for some of these conditions, as possible cause/s of your symptoms.
• The very diagnosis of IC/BPS leads to dozens of unnecessary surgeries on the bladder, with antibiotics, and can actually cause or worsen the very symptoms that urologists call IC/BPS (urgency and frequency and “bladder pain.).” Overuse of antibiotics (used with unnecessary surgeries, like the surgeries on the bladder) can cause a Candida albicans infection, sometimes called Small Intestinal Bacterial Overgrowth (SIBO). (footnote 5) Almost every person of the dozens I’ve interviewed has had intestinal problems, with allergies to many foods, bloating and pain – even a woman in Lesotho who was diagnosed with IC/BPS. The AUA has a long reach, to urologists in many countries, who follow the AUA lead. I can’t give you a definitive test for whether you have Candida albicans infection, but if you’ve had a lot of antibiotics, you likely have it. Candida thrives on sugar, and stopping eating all forms of sugar helped me a great deal, and eventually ended the pain I had with every bite of food. The antibiotics with the dilations of the urethra I had caused allergies to 130 foods.
Again, see Dr. Martin Blaser’s research, mentioned earlier, of the International Human Microbiome Project, overuse of antibiotics has caused many “modern plagues,” which include “… obesity, asthma, allergies, diabetes, and certain forms of cancer.” (Cancer – see Susie’s story) Blaser’s new book is Missing Microbes; How the Overuse of Antibiotics is Fueling Our Modern Plagues , 2014. This is very readable. Blaser: http://martinblaser.com/
• As many as 70% of people diagnosed with IC/BPS have Pelvic floor muscle dysfunction, PFMD, (footnote 6) See James’ story.
• Various pelvic surgeries (hysterectomies, (footnote 7) C-sections, appendectomies, surgeries for bladder prolapse, surgery for endometriosis or removal of the gall bladder and many other pelvic surgeries) can cause damage to organs in the pelvis, like myofascial stricture. See Letter to the AUA, Anne’s story. As many as 44% of women who had a hysterectomy were at risk of being wrongly diagnosed with IC/BPS, (footnote 7) and many undergo unnecessary surgeries and antibiotics, instead of getting what can cure them, physical therapy for myofascial stricture. Hysterectomies and other pelvic surgeries can cause myofascial stricture – which is extremely painful. It bears repeating, surgery is always harmful (footnote 8) and both the surgery and the antibiotic necessary for a surgery are unethical unless the patient is expected to be much more benefited than harmed by the surgery. It appears that no patient is benefitted from the surgeries recommended by the AUA for a diagnosis of IC/BPS, if our survey results, and medical evidence are correct.
• Sensitivity to or allergies to many foods can cause symptoms in the bladder.
• A side effect of pharmaceuticals can be the cause of symptoms - for example Norvasc, which can cause urgency and frequency.
• There can be a bladder infection that the Agar plate (routine urinalysis) does not pick up, such as Chlamydia trachomatis, Ureaplasma urealyticum. A broth culture can be done by www.unitedmedicallab.com and at other labs.
• Hunner’s ulcers in the bladder. The AUA says that this condition should be ruled out before a diagnosis of IC/BPS; actually, however there may be a failure to see the ulcers, and the pain continues until a urologist finally spots them. When they are spotted, the correct surgery can end the pain.
• Chemicals like antiseptics and spermicides
• Viruses like Herpes II virus, (my own case) and Polyoma virus, VZV virus, and Noro virus
• Acidosis of the body
• Lyme disease
• Hormonal problems - the leader of a patient support group says: I do believe that I have organic Bladder Pain Syndrome, BPS – which is not a bladder disease. Hormones are just one part of the many pieces of my puzzle. They did not cause the problem nor cure the problem -- they are just one factor. I believe I have the organic disease (call it what you will) that Dr. Buffington studies -- the neuro-endocrine disorder. I have all of the symptoms for that and I have never heard of a cure -- just trying to keep the symptoms down and hormones help in that (but do not alleviate the symptoms). To say I have a "bladder" disease I believe is just rubbish. Whatever I have is my whole body disease. I hope that makes sense. Dr. C. A. Tony Buffington’s article: https://www.ncbi.nlm.nih.gov/pubmed/15371816 The treatment this woman has used is two-fold:
1) When I began taking bio-identical progesterone around aged 40, this helped to "calm the whole body" as progesterone does, and so all of my symptoms, including bladder symptoms became less severe. (If I would have known about this, I would have tried it much sooner).
2) When I was in my late 40s, my bladder began acting up again with severe symptoms and I realized that because I was in peri-menopause, this likely meant I was decreasing in estrogen. I began also taking bio-identical estrogen, and once again the bladder symptoms decreased to a manageable level.
**Both of these are obtained through a doctor's prescription, and compounded by a pharmacy.
In other words, there are likely many more causes of our symptoms. If our survey results, the medical literature in our Letter to the AUA, the urological research (ICDB Study, ICCTG and ICCRN trials) and other medical research like the Human Microbiome Project are correct, the AUA, and the urologists who follow the AUA Practice Guidelines, are guilty of causing severe harm to people, from these multiple surgeries on the bladder, and the antibiotics that go with surgeries.
THE ABOVE LIST IS BY NO MEANS A COMPLETE LIST OF ALL THE POSSIBLE CAUSES OF THE SYMPTOMS OF URGENCY AND FREQUENCY AND SO-CALLED BLADDER PAIN SYNDROME. If you can find a doctor who practices medicine in a holistic manner, she or he would understand and may be able to help diagnose the real cause/s of your symptoms. The above list of possibilities may be helpful.
Section 3: STILL MORE INFORMATION REGARDING QUESTIONS 1, 2, 3:
1. Question number one is what the AUA recommends for symptoms of urgency and frequency and “bladder pain.”
The Practice Guidelines that the AUA recommends, as we’ve said, are dozens of trial and error surgeries, and the antibiotics required by all surgeries.
2. Does this “treatment” improve patient symptoms? In a word, no.
The bladder is in the pelvis, where there are many other organs, including intestines, the reproductive organs, and so on. So calling these symptoms “bladder pain” is misleading, to say the least, in most cases. And looking at all the causes people have found in the list above, the cause can be anywhere in the body, requiring a holistic diagnosis and the appropriate treatment.
3. Are there known causes and cures for the symptoms urologists call IC/BPS, and what are they?
• Perhaps the biggest failure of modern medicine, including the specialty of urology, has been to basically ignore the issues of prevention of disease and nutrition. Most people, including doctors, would rather not have any diseases, but know little about preventing them, especially with good nutrition.
These key subjects, prevention and nutrition, have been neglected for centuries. In Siddhartha Mukherjee’s book, The Emperor of all Maladies, a Biography of Cancer, (a history of the hypotheses about what causes cancer that underlie the treatments of cancer), there is only one sentence about prevention and nutrition: “…prevention and nutrition are in their infancy.”
Here are 3 estimates of how much nutrition doctors are taught in medical schools:
A National Institutes of Health (NIH) article concludes that of the 97 medical schools surveyed regarding number of hours on nutrition, “Remarkably, less than one-half (41%) of the responding schools provided the minimum 25 h or more recommended by the NAS in 1985 (3). Also surprising was the finding that 17 schools (18%) required only ≤10 h of nutrition instruction.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430660/
US News and World Report seems to have a better grasp of the importance of nutrition regarding health, than medical schools;
https://health.usnews.com/wellness/food/articles/2016-12-07/how-much-do-doctors-learn-about-nutrition :
In recent years, it has become increasingly clear that diet plays a starring role in preventing and treating certain chronic diseases. And physicians are often on the frontlines of counseling patients about how their diets and other lifestyle habits can affect their health and weight – a reality that has gained added importance given the obesity epidemic. And yet, it turns out that only 29 percent of U.S. medical schools offer med students the recommended 25 hours of nutrition education, according to a 2015 report in the Journal of Biomedical Education.”
On average, U.S. medical schools offer only 19.6 hours of nutrition education across four years of medical school, according to a 2010 report in Academic Medicine. In a 2016 study
And the reason for so little instruction on nutrition? “A lack of focus on prevention in medical school.”
• And what is it about prevention of disease and nutrition that might be important for all people, including people diagnosed with IC/BPS?
I worked at Natural History Magazine, The American Museum of Natural History for 25 years. The subject of this Museum is evolution. Most of the exhibits are about the evolution of dinosaurs, mammals, culture, and so on.
However, until I read a new book by the Director of the Human Evolutionary Biology Department at Harvard, Daniel Lieberman, The Story of the Human Body; Evolution, Health and Disease, 2013, the importance of human evolution regarding our health was not a subject I knew much about. (footnote 9) This book doesn’t mention IC/BPS, but gives us a lot to think about regarding the symptoms urologists call IC/BPS, the causes of other diseases, and the role of nutrition and prevention of disease.
Lieberman’s book helps to educate us about our “New, noninfectious disease epidemics,” hypothetically, caused by a “mismatch” between our paleolithic bodies and our new “novel environment.”
That is, our bodies evolve very slowly, and are basically the same as they were 10,000 years ago, during paleolithic times, before agriculture. The list of 50 new epidemics on page 172 of Lieberman’s book, he says, is likely nowhere near the real, much higher number. Lieberman writes about theories that try to explain why these diseases that have always been with us, have now become epidemics. For example, there is much more asthma and more allergies due to exposure to less microorganisms, like germs, and “other environmental factors that disrupt the immune system (which) are certainly more common now, such as pollution and various toxic chemicals in our food, water and air.” (Page. 314).
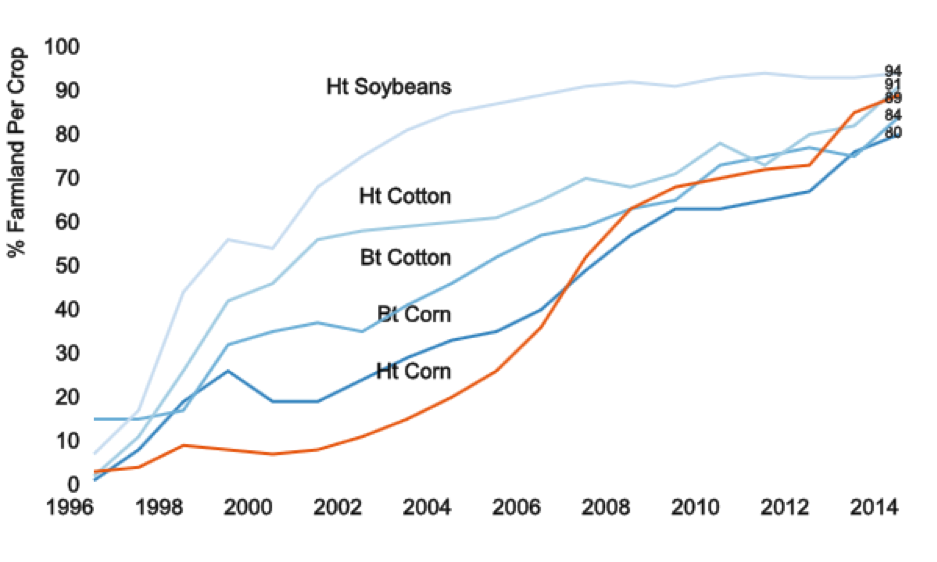
Lieberman does not mention genetically modified food, GMOs, and the herbicide glyphosate, which is used with GMO crops, but glyphosate is one of over 100,000 synthetic, toxic chemicals. When used on any crop, it ends up in the water table, where it effects all people who drink that water, or eat that and other crops irrigated with that water. (footnote 9)
“More than 90% of all soybean, cotton and corn acreage in the U.S. is used to grow genetically engineered crops. Other popular and approved GMO food crops include sugar beets, alfalfa, canola, papaya and summer squash. More recently, apples that don't brown and bruise-free potatoes were also approved by the FDA. It's also instructive to look at permits granted by the United States Department of Agriculture (USDA) and the Food and Drug Administration (FDA) — the American GMO gatekeepers, together with the Environmental Protection Agency…”
http://time.com/3840073/gmo-food-charts/
I submit to you this document:
A strong correlation in the upsurge in use of glyphosate (Monsanto’s Roundup, herbicide used with GMO crops) and the upsurge in 22 noninfectious diseases. Journal of Organic Systems, 9(2), 2014
“Correlation is not cause, but leads to understanding of causation, e.g. “Pearson's Correlation Coefficients show that the probability that glyphosate and/or GMOs are not the cause of these diseases is around a 1 in 10,000 chance.” (In other words, the possibility of this correlation between an upsurge in the use of Roundup and GMOs and an upsurge in 22 noninfectious disease epidemics being wrong is only 1 in 10,000.) The Pearson correlation coefficients are highly significant (10-4) between the percentage of GE corn and soy planted in the US and the increase in 22 noninfectious disease epidemics.
“Evidence is mounting that glyphosate (the synthetic chemical in Roundup, which accompanies GMO crops) interferes with many metabolic processes in plants and animals (including human beings) and glyphosate residues have been detected in both.
“Glyphosate disrupts the endocrine system and the balance of gut bacteria, it damages DNA and is a driver of mutations that lead to cancer.” (The parentheses are mine.)
Journal of Organic Systems, 9(2), 2014,
http://www.organic-systems.org/journal/92/JOS_Volume-9_Number-2_Nov_2014-Swanson-et-al.pdf The parentheses are mine.
Note the dozens of graphs in this journal article, which illustrate this correlation of increasing use of glyphosate/GMOs with and increasing numbers of people with these 22 diseases. This research explains: “A huge increase in the incidence and prevalence of chronic diseases has been reported in the United States (US) over the last 20 years…. In the present study, US government databases were searched for GE crop data, glyphosate application data and disease epidemiological data. Correlation analyses were then performed on a total of 22 diseases in these time-series data sets. The Pearson correlation coefficients are highly significant ( 10-5) between glyphosate applications and hypertension (R = 0.923), stroke (R = 0.925), diabetes prevalence (R = 0.971), diabetes incidence (R = 0.935), obesity (R = 0.962), lipoprotein metabolism disorder (R = 0.973), Alzheimer’s (R = 0.917), senile dementia (R = 0.994), Parkinson's (R = 0.875), multiple sclerosis (R = 0.828), autism (R = 0.989), inflammatory bowel disease (R = 0.938), intestinal infections (R = 0.974), end stage renal disease (R = 0.975), acute kidney failure (R = 0.978), cancers of the thyroid (R = 0.988), liver (R = 0.960), bladder (R = 0.981), pancreas (R = 0.918), kidney (R = 0.973) and myeloid leukaemia (R = 0.878). The significance and strength of the correlations show that the effects of glyphosate and GE crops on human health should be further investigated.
Roundup Exposure Linked To Cancer - Roundup Exposure May Increase The Risk of Non-Hodgkin's Lymphoma. Roundup Cancer Lawsuit:
http://roundupcompensation.com/?gclid=CKSt2-aPnckCFYGXgQodkxkGfQ
Another example of a synthetic chemical, the most used herbicide in the US, Atrazine, and research showing the hormone disruption caused by this chemical – female frogs becoming male frogs, vice versa, and then the two mating: A New Yorker Magazine article: atrazine, the most used herbicide in the US, regarding the researcher, Syngenta, corporation that sells Atrazine, the effect on amphibians and likely humans. “A Valuable Reputation,”
http://www.newyorker.com/reporting/2014/02/10/140210fa_fact_aviv?currentPage=all
When will our government (USDA, FDA) stop approving these corporate products, like GMOs and glyphosate, which in effect makes us all human experimental subjects? It reminds me of the medical experiments done on people in concentration camps under the Nazis.
Personally, I travel to farms within an hour of our home to get fruits and vegetables where there are no toxins used to grow those plants, in soil that is not depleted of the nutrients we need to be healthy.
• With respect to human evolutionary biology, new epidemics and their causes, how might this shed light on the symptoms urologists call IC/BPS?
The President of the Canadian Urological Association, Professor of Urology at Queen’s University in Canada, Dr. J Curtis Nickel, and colleagues, have studied a group of patients diagnosed with IC/BPS and discovered that they have “associated non bladder syndromes and conditions (which) must be addressed as well as the urological issues, “…by the urologist, the family physician and in many cases by specific specialists working collaboratively to treat the ‘whole patient.’” Dr. Nickel maintains that if these associated conditions are not diagnosed and treated, “the patient will not be helped.” (footnote 10)
These conditions, says Dr. Nickel, “ include IBS (59% of a studied patient group), Fibromyalgia (59%), chronic fatigue (18%), diseases which are Genito-Urinary (71%), Neurogenic (35%), Hematologic, blood,(18%), Psychiatric, depression (35%), Gastro Intestinal, stomach, intestines, (88%), ENT, ears, nose and throat (41%), Allergic/immune system (47%), MSK - Medullary Sponge Kidney, leading to blood in the urine, kidney stones, urinary tract infections, (82%) Dermatological, skin (6%), Cardiovascular, 29%, Pulomnary, lungs (88%) and/or Endocrinologic – hormone issues- (47%). Underlining is mine. (footnote 11)
The question I asked Dr. Nickel is how many of these conditions might be caused by overuse of antibiotics, by food laden with pesticides, glyphosate and other herbicides and the more than 100,000 other synthetic chemicals now sold?
Dr. Nickel responds to this question, 3/1/18: As far as your query in regard to antibiotics causing many of the associated conditions, there is no proof one way or another. However we do know that these conditions are increasing and very well may have an environmental etiology. Certainly our food in terms of diet, environmental pollutants and overuse of antibiotics may be implicated. (etiology means “the cause, set of causes, or manner of causation of a disease or condition”)
I reply: Re: antibiotics, we know that the AUA Guidelines involve a lot of surgeries, each with an antibiotic, and we have known since the public use of antibiotics, in the 1940s, that the result is the overgrowth of Candida albicans – and now we know how these antibiotics effect the whole microbiome of the body. (Martin Blaser, NYU Langone, the international human microbiome project etc.).
Dr. Nickel has been very generous with his time, in reanalyzing our survey data, and in many emails. If you want to thank him, you can find his email online, at J Curtis Nickel, urologist.
• My story (Kay Zakariasen), and survey results:
I, like Susie and every other person I’ve spoken to, and likely all 1628 women and the men who responded to our survey, just want to help other people avoid going through what we’ve been through. There is no profit for any of us, except knowledge and the ability to protect our own and our family’s health as much as possible.
• National Women’s Health Network Newsletter, 2009: My story and results of our survey:
https://www.nwhn.org/the-treatment-and-mistreatment-of-chronic-urgency-and-frequency-gathering-womens-experiences-about-interstitial-cystitis/
• Prevention Magazine Article:
http://www.cystitispatientsurvey.com/prevention1t.jsp
Please note that there is a “next page” prompt in the upper right hand corner of each page. on our original website so that you can read the entire article. Zakariasen, Kay, “Cystitis: Getting Off the Treatment Treadmill”, Prevention Magazine, 1983; April, pp. 104-9.
Twenty five people who read this article sent me letters, and became my first contacts with other people diagnosed with cystitis or IC. One woman said “Kay, I’ve been butchered.” This pretty much sums up the content of all of these letters and conversations with these people.
• How long have urologists been operating on women’s bladder, nervous system, vagina, for symptoms of urgency and frequency and pelvic pain? And how many women and female children? A testimony to the risks of surgery, and the importance of prevention, nutrition, and a holistic diagnosis and treatment of our painful symptoms:
The Historical Context, since 1871, of the current American Urological Association Practice Guidelines for two symptoms – urgency and frequency and “bladder pain,” currently called interstitial cystitis/bladder pain syndrome, IC/BPS by the AUA:
The following surgeries, since 1871, would have caused chronic pain, and maimed and killed many of the women that experienced them and without antibiotics (before 1940) would have caused death in many, from infection. At the end of this list are 6 different ways to remove the bladder – which thousands (maybe more) of women have endured, with no benefit. Removal of the bladder is still being done, often after severe hydrodistentions are done by urologists, severely reducing the capacity of the bladder. While it is known that every urologist does their own version of hydrodistention, some 3 hours at high pressure, and this is recommended against in the Practice Guidelines, the AUA does nothing to stop this. See Susie’s story, and since removal of the bladder is part of the Guidelines, there must be thousands more stories like hers.
27 surgeries (Sant/Christmas):
INTERSTITIAL CYSTITIS, Ed. Grannum Sant, Lippincott-Raven Publishers, Philadelphia, 1997, Chapter 1, “Historical Aspects of Interstitial Cystitis,” 1-7, Table 4: Review of surgical treatments for IC, p. 7:
1. Formation of vesico-vaginal fistula, Tait, 1870 (footnote 3)
2. Local debridement, Fenwick, 1896 (5)
3. Local excision of ulcers, Hunner, 1915 (7)
4. Fulguration of ulcers, Kreutzmann, 1922 (12)
5. Dental extraction, Frontz, 1928 (14)
6. Cystodistension under general anaesthesia, Bumpus, 1930 (16)
7. Presacral neurectomy, Pieri, 1930 (23)
8. Cordotomy, Grant, 1931 (85)
9. Augmentation enterocystoplasty, Sebening, 1932 (25)
10. Excision of superior hypogastric plexus, Douglass, 1934 (27)
11. Cystoscopic ulcer resection, Sears, 1936 (30)
12. Transvesical alcohol injection, Folsom and O’Brien,1937 (not 22, but 33+34)
13. Bilateral ureterosigmoidostomy, Counselor, 1937 (34)
14. Sensory denervation by local sympathectomy, Scott & Schroeder, 1938 (28)
15. Subtotal cystectomy & substitution enterocystoplasty, (Folsom et. al.)1940 (36)
16. Cystoscopic hydrocortisone infiltration, Johnston, 1956 (48)
17. Sacral (S l-3) root rhizotomy,Franksson, 1957 (50)
18. Sacral (S 2-3) root rhizotomy, Bohn & Franksson, 1957 (50)
19. Sacral (S 3) root rhizotomy, Milner & Garlick, 1957 (51)
20. Subtotal cystectomy & colocystoplasty, Gil-Vernet et. al, 1960 (22)
21. Cystocystoplasty, Warwick & Ashken, 1967 (86)
22. Total cystectomy and ileal conduit diversion, Worth & Warwick, 1973 (87)
23. Total cystectomy & ileal conduit diversion, Jacobo et al., 1974 (88)
24. Neodymium YAG-laser therapy, Shanberg et al., 1985 (89)
25. Laparoscopic laser destruction of nerve plexus, Gillespie, 1994 (90)
26. Total bladder replacement by ileocolic segment, Bejany & Politano, 1995 (91)
27. Total bladder replacement by Kock pouch, Christmas